Abstract
Purpose
The purpose of this study was to evaluate the validity and reliability of the Turkish version of the Nijmegen Cochlear Implant Questionnaire (Tr-NCIQ) and reveal the demographic factors contributing to the outcomes.
Methods
A group of 118 cochlear implant users aged between 18 and 70 years filled the Tr-NCIQ and the Turkish Hearing Handicapped Inventory for Adults (the Tr-HHI-Adult) via electronic survey. Cross-cultural adaptation of the Tr-NCIQ was performed. The reliability and validity of the questionnaire were evaluated utilizing internal consistency coefficient, split-half method, and predictive validity.
Results
The overall Cronbach’s alpha coefficient of the scale was 0.91, and the Spearman-Brown coefficient was 0.91. A moderately significant and negative correlation was present between the basic sound perception, speech production, self-esteem, activity, and social interactions subdomain scores and the HHI-Adult scores. Patients with post-lingual onset of hearing loss had significantly better results than those with pre-lingual onset, in the advanced sound perception subdomain. In addition, bilateral cochlear implant users had better results than the unilateral and bimodal users in the speech production subdomain and then the bimodal users in the self-esteem subdomain. There was no effect of age, duration of implant use, age at implantation, and the daily usage of cochlear implant (CI) on the quality-of-life outcomes.
Conclusion
The Tr-NCIQ is a reliable and valid tool to evaluate the subjective quality of life in CI users. In addition, as a standardized instrument, it can be easily self-administered both in clinical practice and for research purposes.
Similar content being viewed by others

Introduction
Cochlear implantation is a well-accepted treatment method to compensate for severe to profound sensorineural hearing loss [1]. The improvements in both speech performance and quality of life (QoL) in cochlear implant (CI) users are considered two main outcomes for the effectiveness and success of a CI [2, 3]. CI technology provides easy access to speech sounds by providing adequate environmental stimulation, leading to an improvement in the speech understanding of its users [4]. The speech performance improvement thanks to the use of CI directly reduces or eliminates the adverse effects of hearing loss on self-esteem, daily-life activities, and social functioning [5].
Despite technological advances in surgical techniques, electrode designs, sound processors, programming methods, and even rehabilitation recently, CI users can differ in terms of speech understanding and QoL outcomes [3]. Individual variability such as age [6], cognitive skills [7], the duration of the auditory deprivation [8], the use of hearing aid before CI [9, 10], age of implantation [9, 11], and low-frequency residual hearing [12] can affect both access to sounds and QoL after implantation. The effects of these factors on auditory and language development have been evaluated by behavioral test methods such as a response to environmental sounds (13), speech recognition threshold (SRT) [14], speech recognition score (SRS) [15], and sentence tests in noise [16]. To assess the impact and effectiveness of CI on QoL and to examine the relationship between individual factors and different psycho-social domains in terms of CI usage, different self-reported QoL instruments were used [17,18,19].
The subjective benefits of a cochlear implant can be determined using generic-based or disease-specific health-related QoL instruments in nature. Generic-based tools were developed to evaluate a wide range of health problems not specific to the effects of a particular disease itself or the treatment process of this disease on QoL. For example, Patient Quality of Life Form [20], Health Utilities Index [21], Center of Epidemiologic Studies-Depression Scale [22], and Glasgow Benefit Inventory (GBI) [23] are generic-based instruments commonly used to assess health-related QoL in CI users. Although these instruments provide valuable information about various aspects of cochlear implantation, as they cannot evaluate the effects of CI on auditory functions and/or QoL as a whole, several reports have recommended the use of different combinations of them [24, 25]. However, instruments specific to QoL assessment associated with a particular disease and/or treatment in a particular population provide a more accurate and more effective information. For this reason, Hinderink, Krabbe and Broek [21] developed the Nijmegen Cochlear Implant Questionnaire (NCIQ), a disease-specific instrument to assess both speech and health-related QoL issues for CI users [17]. Additionally, on NCIQ reports, the cost–benefit consequences of the CI intervention as well as the effects of technological developments and the auditory rehabilitation process on the QoL of adult CI users were evaluated in detail.
It is necessary to scientifically show that an instrument is an internationally valid and reliable tool to determine the language/culture-specific variables. The NCIQ, providing valuable information in determining the needs and success levels of adult CI implant users both in clinical and real-life conditions, has been adapted to different languages, including Chinese [26], Spanish [27], Italian [28], and Brazilian-Portuguese [29], and psychometrically analyzed.
No measurement tool evaluates the speech and QoL variations of adult CI users in Turkey to date. Therefore, the main purpose of this study is to adapt the NCIQ into the Turkish language and to determine the reliability and predictive validity of the Turkish version of the NCIQ (the Tr-NCIQ) as a quantifiable self-assessment health-related QoL in adult CI users. It was hypothesized that the Tr-NCIQ is both a reliable and valid instrument.
Methods
This study included 118 CI users (62 females and 56 males) aged between 18 and 70 years. All participants had at least 6 months of CI experience. Demographic data are provided in Table 1. Descriptive statistics are presented in Table 2.
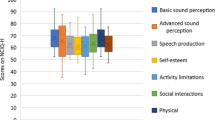
The NCIQ was constructed in three domains (physical, social and psychological) including six subdomains: basic sound perception, advanced sound perception, speech production, self-esteem, activity, and social interactions. Each subdomain covers ten items. The NCIQ, prepared in a 5-point Likert form, consists of a total of 60 items. [17]. The first 55 items include “never (1), sometimes (2), regularly (3), usually (4), always (5),” and the remaining 5 items include “no (1), poor (2), moderate (3), good (4), fairly good (5)” response options. The sixth response category “not applicable (N/A)” is available in case the item is not suitable for the patients. To obtain a total score for each subdomain, participant’s responses are categorized as (1 = 0, 2 = 25, 3 = 50, 4 = 75, and 5 = 100), then the scores from each 10-item subdomain are summed, and divided by the number of answered items. A higher score on the questionnaire shows a better QoL.
Cross-cultural adaptation of the NCIQ (with the courtesy of Dr. Hinderink et al.) was performed using the combination of back-translation and committee methods following cultural guidelines [30]. The professional translators conducted the two-way translations (English to Turkish and Turkish to English) for semantic evaluation of the Tr-NCIQ. Two experts, one of whom is a specialist in linguistics, evaluated these two translations and offered necessary arrangements. Then, the two experts in the field of audiology examined the suitability of the items. Both audiologists agreed that 58 of the 60 items were appropriate. The fit index was calculated as 97%. The other two items were changed as two audiologists suggested. In a pilot study, 19 CI users filled the questionnaire to evaluate the comprehensibility of the items and the scope of the Turkish translation. After minor corrections, the Tr-NCIQ took its final form.
The Turkish short version of the Hearing Handicap Inventory for Adults (the Tr-HHI-Adult) [31] was used to evaluate the predictive validity of the Tr-NCIQ. Participants completed the Tr-NCIQ and Tr-HHI-Adult as an electronic survey. The survey link was shared on social media to reach associations and groups of CI users.
Ethics committee approval was received from the Başkent University Institutional Review Board and Ethics Committee (Protocol No: KA18/399). The purpose and terms of participation in the study was explained and informed consent was obtained from all participants by checking the option “I agree to voluntarily participate in this study”.
Statistical analysis
Statistical Package for the Social Sciences (SPSS) version 25.0 (IBM Corp, Armonk, NY, USA) was used. The Kolmogorov–Smirnov and Levene tests were used to evaluate the normality distribution and the homogeneity of the variances, respectively. The reliability of the Tr-NCIQ was calculated using the internal consistency coefficient and split-half methods. To predict the validity, the relationship between the subdomain scores of Tr-NCIQ and Tr-HHI-Adult was evaluated with Spearman’s correlation coefficient. Independent samples’ t-test was used to compare the Tr-NCIQ scores of pre- and post-lingual CI users. The subdomain scores for bimodal, bilateral, and unilateral CI usage were compared with one-way ANOVA. Spearman’s r correlation between subdomain scores of Tr-NCIQ and age of implantation/duration of implant use/duration of hearing aid use was examined. All statistical tests are conducted at the α = 0.05 significance level.
Results
Both the overall Cronbach alpha and the Spearman-Brown coefficients were 0.91. The Cronbach’s alpha coefficients for each subdomain are presented in Table 3. Cronbach’s alpha coefficient of the subdomains was above 0.70, indicating good internal consistency.
The relationship between the HHI-Adult and the Tr-NCIQ scores was examined on 43 individuals to evaluate the validity of the questionnaire. No significant correlation was found between the scores of advanced sound perception subdomain and HHI-Adult scores. A moderately significant and negative correlation was present between the basic sound perception, speech production, self-esteem, activity, and social interactions subdomain and the HHI-Adult scores (Table 4). A significant and negative correlation indicates a tendency that the quality of life decreases as the hearing impairment increases (Fig. 1).
The Tr-NCIQ scores were evaluated in terms of demographic and descriptive statistics data. The scores of each subdomain were analyzed concerning the onset of hearing loss. The independent samples t test indicated a statistically significant difference between the pre- and post-lingual groups only in the advanced sound perception subdomain [t (113) = -2.19, p = 0.030] (Table 5). The 95% confidence interval for the scores in terms of pre- and post-lingual scores are presented in Fig. 2. One-way ANOVA test revealed a significant difference between speech production and self-esteem subdomain scores in terms of bimodal, bilateral and unilateral CI use [F (2;111) = 6.54, p = 0.002; F (2.111) = 3.47, p = 0.034, respectively] (Table 6). According to the Tukey HSD test, bilateral implant users differ in speech production subdomain compared to other groups (p = 0.02 for bilateral and bimodal comparison; p = 0.010 for bilateral and unilateral comparison). Additionally, a significant difference existed between the self-esteem subdomain scores of bilateral and bimodal CI users (p = 0.026). Spearman’s r test results did not reveal a significant relationship between the subdomains of the Tr-NCIQ and any variable such as duration of implant use, the age of implantation, and the daily use of CI.
Discussion
In this study, the psychometric properties of the Tr-NCIQ and the effects of demographic variables in adult CI users were examined. The results indicated good internal consistency and moderate predictive validity.
Both overall Cronbach’s α coefficient and the split-half reliability of the Tr-NCIQ were 0.91. The Cronbach’s α coefficients for the subdomains were above 0.70. The lowest coefficient was the social interactions subdomain with 0.70, and the activity subdomain had the highest coefficient: 0.90. These findings are similar to the original study [17], Spanish [27], Italian [28], and Brazilian [29] translations. Additionally, a high degree of internal consistency indicates that Tr-NCIQ is a reliable tool for determining the benefit from a CI.
The NCIQ is based on the classical test theory concept, where each item is considered equally important. There are no weighted scores in the NCIQ, and every step between the response categories is considered equal. NCIQ has a concept consisting of ten items in each subdomain [17]. In evaluating the quality of life of CI users, the number of items in the subdomains are wide enough to cover all life activities, which, enables the whole quality of life of CI users to be questioned reliably. However, it can be restrictive for the validity study of the questionnaire. In particular, the necessity of reaching a large number of participants to perform a factor analysis (FA), for example, the need for at least 10 times the number of items for 60 items limited the conduct of the FA in our study. A confirmatory factor analysis with 118 participants to evaluate the construct validity in our study revealed no clear pattern as in the Spanish version [27]. Therefore, to estimate the validity, we examined the relationship between Tr-HHI-Adult and Tr-NCIQ scores. The fact that there was a moderately significant and negative relationship between the HHI-Adult scores and the scores of all subdomains, except for advanced sound perception indicates that the quality of life tends to decrease as hearing loss increases. This also shows the indication of the predictive validity of the Tr-NCIQ. However, further studies with a large population are needed to support the validity of the questionnaire.
The analysis of the relationship between demographic data and Tr-NCIQ sub-domains showed that the use of CI was not associated with the duration of implant use, age at implantation, and daily implant use. Although we cannot generalize the results, the Tr-NCIQ gave us some distinct information regarding the impact of CI use on quality of life overall. First, CI users with the post-lingual onset of hearing loss had significantly higher scores, which indicates a better quality of life, than those with pre-lingual onset, in the advanced sound perception subdomain. Second, bilateral CI users had higher scores than unilateral and bimodal users in the speech production subdomain and then the bimodal users in the self-esteem subdomain. Although the number of bilateral CI users was small in this study, differences in speech production subdomain scores of bilateral CI users compared to those of bimodal and unilateral CI users showed both the reliability of the questionnaire and the positive effects of bilateral CI use on QoL. These data are consistent with the new reports [32]. Additionally, the highest scores in Tr-NCIQ were obtained in activity (in social domain) and basic sound perception (in physical domain), respectively. Advanced sound perception and speech production sub-domains (in physical domain) followed them. Also, previous reports have shown that the use of CI positively affects the quality of life, especially in these areas. [33,34,35]. Evaluating all these Tr-NCIQ results together showed that using a disease-specific measurement tool instead of a generic-based provides a more accurate and effective information about the issue related with QoL.
Regarding the administration of the Tr-NCIQ, although the number of items was too much, the participants gave positive feedback that the questions were easy to understand and many aspects of their lives were well questioned.
The evaluation of the quality of life, employing the NCIQ pre- and post-CI has been examined in detail in previous studies [9, 25, 32], where a significant increase in post-implantation NCIQ scores has been reported. Since this study coincided with the COVID-19 pandemic, participants’ quality of life before and after implantation was not examined with the Tr-NCIQ and was not supported by objective audiological outcomes either. This situation can be considered a shortcoming of the current study. However, the adaptation of the NCIQ into the Turkish language and the results showing that the Tr-NCIQ has high reliability and moderate predictive validity should then be considered as the first step to evaluate the relationship between the audiological profiles and quality of life of Turkish CI users.
Conclusion
The current findings support that the Tr-NCIQ is a reliable and valid tool to evaluate the subjective QOL in CI users. Additionally, as a standardized instrument, it can be easily self-administered both in clinical practice and for research.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Nadol JB Jr, Young YS, Glynn RJ (1989) Survival of spiral ganglion cells in profound sensorineural hearing loss: implications for cochlear implantation. Ann Otol Rhinol Laryngol 98:411–416. https://doi.org/10.1177/000348948909800602
Távora-Vieira D, Marino R, Acharya A, Rajan GP (2015) The impact of cochlear implantation on speech understanding, subjective hearing performance, and tinnitus perception in patients with unilateral severe to profound hearing loss. Otol Neurotol 36:430–436. https://doi.org/10.1097/MAO.0000000000000707
Sousa AF, Couto MIV, Martinho-Carvalho AC (2018) Quality of life and cochlear implant: results in adults with postlingual hearing loss. Braz J Otorhinolaryngol 84:494–499. https://doi.org/10.1016/j.bjorl.2017.06.005
Távora-Vieira D, Marino R (2019) Re-training the deaf ear: Auditory training for adult cochlear implant users with single sided deafness. Cochlear Implants Int 20:231–236. https://doi.org/10.1080/14670100.2019.1603652
Forli FT, Giuntini G, Bellelli G, Fortunato S, Bruschini S, Barillari L, Berrettini MR (2017) Cochlear implant in prelingually deafened oralist adults: speech perception outcomes, subjective benefits and quality of life improvement. Acta Otorhinolaryngol Ital 37:416. https://doi.org/10.14639/0392-100X-1493
Straatman LV, Huinck WJ, Langereis MC, Snik AF, Mulder JJ (2014) Cochlear implantation in late-implanted prelingually deafened adults: changes in quality of life. Otol Neurotol 35:253–259. https://doi.org/10.1097/MAO.0b013e3182a4758e
Völter C, Götze L, Dazert S, Falkenstein M, Thomas JP (2018) Can cochlear implantation improve neurocognition in the aging population? Clin Interv Aging 13:701–712. https://doi.org/10.2147/CIA.S160517
del Mar Medina MP, Polo R, Gutierrez A, Muriel A, Vaca M, Perez C, Cordero A, Cobeta I (2017) Cochlear implantation in postlingual adult patients with long-term auditory deprivation. Otol Neurotol 38:248–252. https://doi.org/10.1097/MAO.0000000000001257
Baser B, Patidar M, Surana PA (2020) Study to determine various factors influencing auditory outcomes in paediatric cochlear implantation. Indian J Otolaryngol Head Neck Surg 72:453–456. https://doi.org/10.1007/s12070-020-01900-2
Çolak M, Bayramoğlu İ, Tutar H, Altınyay Ş (2019) Benefits on language development and auditory perception performance of using a contralateral hearing aid in cochlear implanted children. ENT Updates 9:191–198. https://doi.org/10.32448/entupdates.601175
Gaurav V, Sharma S, Singh S (2020) Effects of age at cochlear implantation on auditory outcomes in cochlear implant recipient children. Indian J Otolaryngol Head Neck Surg 72:79–85. https://doi.org/10.1007/s12070-019-01753-4
Yüksel M, Meredith MA, Rubinstein JT (2019) Effects of low frequency residual hearing on music perception and psychoacoustic abilities in pediatric cochlear implant recipients. Front Neurosci 13:924. https://doi.org/10.3389/fnins.2019.00924
Moon IJ, Kim EY, Chu H, Chung WH, Cho YS, Hong SH (2011) A new measurement tool for speech development based on Ling’s stages of speech acquisition in pediatric cochlear implant recipients. Int J Pediatr Otorhinolaryngol 75:495–499. https://doi.org/10.1016/j.ijporl.2011.01.003
Mahmoud AF, Massa ST, Douberly SL, Montes ML, Ruckenstein MJ (2014) Safety, efficacy, and hearing preservation using an integrated electro-acoustic stimulation hearing system. J Otol Neurotol 35:1421–1455. https://doi.org/10.1097/MAO.0000000000000422
Alnıaçık A, Ferda A (2019) The effects of adaptive directional microphone on auditory evoked cortical P300 response and speech performance in cochlear implant users. Int J Audiol 58:861–868. https://doi.org/10.1080/14992027.2019.1637028
Dornhoffer JR, Reddy P, Meyer TA, Schvartz-Leyzac KC, Dubno JR, McRackan TR (2021) Individual differences in speech recognition changes after cochlear implantation. JAMA Otolaryngol Head Neck Surg 147:280–286. https://doi.org/10.1001/jamaoto.2020.5094
Hinderink JB, Krabbe PF, Van Den Broek P (2000) Development and application of a health-related quality-of-life instrument for adults with cochlear implants: the Nijmegen cochlear implant questionnaire. Otolaryngol Head Neck Surg 123:756–765. https://doi.org/10.1067/mhn.2000.108203
McRackan TR, Hand BN (2019) Cochlear implant quality of life development consortium, Velozo CA, Dubno JR. Cochlear implant quality of life (CIQOL): development of a profile instrument (CIQOL-35 Profile) and a global measure (CIQOL-10 Global). J Speech Lang Hear Res 62:3554–3563. https://doi.org/10.1044/2019_JSLHR-H-19-0142
King N, Nahm EA, Liberatos P, Shi Q, Kim AH (2014) A new comprehensive cochlear implant questionnaire for measuring quality of life after sequential bilateral cochlear implantation. Otol Neurotol 35:407–413. https://doi.org/10.1097/MAO.0000000000000229
Mo B, Lindbæk M, Harris S (2005) Cochlear implants and quality of life: a prospective study. Ear Hear 26:186–194. https://doi.org/10.1097/00003446-200504000-00006
Andries E, Gilles A, Topsakal V, Vanderveken O, Van de Heyning P, Van Rompaey V, Mertens G (2021) The impact of cochlear implantation on health-related quality of life in older adults, measured with the health utilities index mark 2 and mark 3. Eur Arch Otorhinolaryngol. https://doi.org/10.1007/s00405-021-06727-3
Boi R, Racca L, Cavallero A et al (2012) Hearing loss and depressive symptoms in elderly patients. Geriatr Gerontol Int 12:440–445. https://doi.org/10.1111/j.1447-0594.2011.00789.x
Sanchez-Cuadrado IL, Perez-Mora L, Muñoz R, Javier EG (2015) Reliability and validity of the Spanish glasgow benefit inventory after cochlear implant surgery in adults. Eur Arch Otorhinolaryngol 272:333–336. https://doi.org/10.1007/s00405-013-2844-y
Maillet CT, Jordan RS (1995) Change in the quality of life of adult cochlear implant patients. Ann Otol Rhinol Laryngol 165:31–48
Harris JPA, John P, Novak R (1995) An outcomes study of cochlear implants in deaf patients: audiologic, economic, and quality-of-life changes. Arch Otorhinolaryngol-Head Neck Surg 121:398–404. https://doi.org/10.1001/archotol.1995.01890040024004
Dong RJ, Liu B, Peng XX, Chen XQ, Gong SS (2010) Analysis of reliability and validity of the Chinese version of Nijmegen cochlear implant questionnaire. Zhonghua er bi yan hou tou Jing wai ke za zhi = Chin J Otorhinolaryngol Head Neck Surg 45:818–823
Sanchez-Cuadrado I, Gavilan J, Perez-Mora R, Muñoz E, Lassaletta L (2015) Reliability and validity of the Nijmegen cochlear implant questionnaire in Spanish. Eur Arch Otorhinolaryngol 272:1621–1625. https://doi.org/10.1007/s00405-014-2983-9
Ottaviani F, Iacona E, Sykopetrites V, Schindler A, Mozzanica F (2016) Cross-cultural adaptation and validation of the Nijmegen Cochlear Implant Questionnaire into Italian. Eur Arch Otorhinolaryngol 273:2001–2007. https://doi.org/10.1007/s00405-015-3765-8
Santos NPD, Couto MIV, Martinho-Carvalho AC (2017) Nijmegen Cochlear Implant Questionnaire (NCIQ): translation, cultural adaptation, and application in adults with cochlear implants. In: Codas, vol 29. Sociedade Brasileira de Fonoaudiologia, Brazil
Brislin RW (1970) Back-translation for cross-cultural research. J Cross Cult Psychol 1:185–216. https://doi.org/10.1177/135910457000100301
Aksoy S, Aslan F, Köse A (2020) İşitme engeli ölçeği–erişkin: uzun ve tarama formlarının Türkçe sürümünün geçerliğinin ve güvenirliğinin incelenmesi. KBB-Forum 19:169–181
Sivonen V, SinkkonenWillberg STT et al (2021) Improvements in hearing and in quality of life after sequential bilateral cochlear implantation in a consecutive sample of adult patients with severe-to-profound hearing loss. J Clin Med 10:2394. https://doi.org/10.3390/jcm10112394
Damen GW, Beynon AJ, Krabbe PF, Mulder JJ, Mylanus EA (2007) Cochlear implantation and quality of life in postlingually deaf adults: long-term follow-up. Otolaryngol Head Neck Surg 136:597–604. https://doi.org/10.1016/j.otohns.2006.11.044
Klop WM, Briaire JJ, Stiggelbout AM, Frijns JH (2007) Cochlear implant outcomes and quality of life in adults with prelingual deafness. Laryngoscope 117:1982–1987. https://doi.org/10.1097/MLG.0b013e31812f56a6.28
Louza J, Hempel JM, Krause E, Berghaus A, Müller J, Braun BT (2017) Patient benefit from cochlear implantation in single-sided deafness: a 1-year follow-up. Eur Arch Otorhinolaryngol 27:2405–2409. https://doi.org/10.1007/s00405-017-4511-1
Acknowledgements
The authors express their deep appreciation to all those who participated in this study. This study was previously presented as an “oral presentation” at X. National Audiology and Speech Disorders Congress.
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by AA, EÇ and OÖ. The first draft of the manuscript was written by AA and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. Conceptualization: AA, EÇ and OÖ; methodology: AA, EÇ and OÖ; formal analysis and investigation: AA, EÇ, OÖ; writing—original draft preparation: AA; writing—review and editing: AA, EÇ, OÖ; resources: AA, OÖ; supervision: AA, EÇ.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial or proprietary interests in any material discussed in this article.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by Başkent University Institutional Review Board and Ethics Committee (Protocol No: KA18/399).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alnıaçık, A., Çakmak, E. & Öz, O. Cross-cultural adaptation of the Nijmegen cochlear implant questionnaire into Turkish language: validity, reliability and effects of demographic variables. Eur Arch Otorhinolaryngol 279, 2175–2182 (2022). https://doi.org/10.1007/s00405-021-07191-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-07191-9