Abstract
Purpose
To determine the usefulness of the Health Utilities Index (HUI) in older cochlear implant (CI) recipients, the primary aims were: (1) to assess health-related quality of life (HRQoL), measured with HUI, in older CI candidates while comparing with age- and gender-matched normal-hearing controls; (2) to compare HRQoL after CI with the pre-operative situation, using HUI and the Nijmegen cochlear implant questionnaire (NCIQ). The difference between pre- and postoperative speech intelligibility in noise (SPIN) and in quiet (SPIQ) and the influence of pre-operative vestibular function on HRQoL in CI users were also studied.
Methods
Twenty CI users aged 55 years and older with bilateral severe-to-profound postlingual sensorineural hearing loss and an age- and gender-matched normal-hearing control group were included. HRQoL was assessed with HUI Mark 2 (HUI2), HUI Mark 3 (HUI3) and NCIQ. The CI recipients were evaluated pre-operatively and 12 months postoperatively.
Results
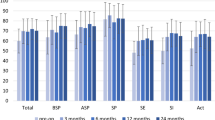
HUI3 Hearing (p = 0.02), SPIQ (p < 0.001), SPIN (p < 0.001) and NCIQ (p = 0.001) scores improved significantly comparing pre- and postoperative measurements in the CI group. No significant improvement was found comparing pre- and postoperative HUI3 Multi-Attribute scores (p = 0.07). The HUI3 Multi-Attribute score after CI remained significantly worse (p < 0.001) than those of the control group. Vestibular loss was significantly related to a decrease in HUI3 Multi-Attribute (p = 0.037) and HUI3 Emotion (p = 0.021) scores.
Conclusion
The HUI is suitable to detect differences between normal-hearing controls and CI users, but might underestimate HRQoL changes after CI in CI users over 55.



Similar content being viewed by others
Availability of data and material
To protect study participant privacy, data cannot be shared openly. The public availability of data was not included in the ethics approval of this study. The datamanagement part of the study protocol states that raw participant data can only be accessed by the principal investigators and cannot be shared or given to anyone outside the study team.
Code availability
Not applicable.
References
WHO (2018) WHO global estimates on prevalence of hearing loss Prevention of Deafness. World Health Organisation, Geneva
D’haese PSC, De Bodt M, Van Rompaey V, Van de Heyning P (2018) Awareness of hearing loss in older adults: results of a survey conducted in 500 subjects across 5 European countries as a basis for an online awareness campaign. INQUIRY: The Journal of Health Care Organization, Provision, and Financing 55. https://doi.org/https://doi.org/10.1177/0046958018759421
Buchman CA, Fucci MJ, Luxford WM (1999) Cochlear implants in the geriatric population: benefits outweigh risks. Ear Nose Throat J 78(7):489–494
Agrawal Y, Pineault KG, Semenov YR (2018) Health-related quality of life and economic burden of vestibular loss in older adults. Laryngosc Invest Otolaryngol 3(1):8–15. https://doi.org/10.1002/lio2.129
Claes AJ, Van de Heyning P, Gilles A, Van Rompaey V, Mertens G (2018) Cognitive performance of severely hearing-impaired older adults before and after cochlear implantation: preliminary results of a prospective, longitudinal cohort study using the RBANS-H. Otol Neurotol 39(9):e765–e773. https://doi.org/10.1097/mao.0000000000001936
Lenarz M, Sonmez H, Joseph G, Buchner A, Lenarz T (2012) Cochlear implant performance in geriatric patients. Laryngoscope 122(6):1361–1365. https://doi.org/10.1002/lary.23232
Zwolan AT, Henion AK, Segel AP, Runge AC (2014) The role of age on cochlear implant performance, use, and health utility: a multicenter clinical trial. Otol Neurotol 35(9):1560–1568. https://doi.org/10.1097/MAO.0000000000000583
Claes AJ, Van de Heyning P, Gilles A, Hofkens-Van den Brandt A, Van Rompaey V, Mertens G (2018) Impaired cognitive functioning in cochlear implant recipients over the age of 55 years: a cross-sectional study using the repeatable battery for the assessment of neuropsychological status for hearing-impaired individuals (RBANS-H). Front Neurosci 12:580. https://doi.org/10.3389/fnins.2018.00580
Völter C, Götze L, Dazert S, Falkenstein M, Thomas JP (2018) Can cochlear implantation improve neurocognition in the aging population? Clin Interv Aging 13:701–712
Jayakody PDM, Friedland LP, Nel NE, Martins DR, Atlas RM, Sohrabi RH (2017) Impact of cochlear implantation on cognitive functions of older adults: pilot test results. Otol Neurotol 38(8):e289–e295. https://doi.org/10.1097/MAO.0000000000001502
Mosnier I, Vanier A, Bonnard D, Lina-Granade G, Truy E, Bordure P, Godey B, Marx M, Lescanne E, Venail F, Poncet C, Sterkers O, Belmin J (2018) Long-term cognitive prognosis of profoundly deaf older adults after hearing rehabilitation using cochlear implants. J Am Geriatr Soc 66(8):1553. https://doi.org/10.1111/jgs.15445
Theofilou P (2013) Quality of life: definition and measurement. Eur J Psychol 9(1):150–162. https://doi.org/10.5964/ejop.v9i1.337
Hinderink JB, Krabbe PF, Van Den Broek P (2000) Development and application of a health-related quality-of-life instrument for adults with cochlear implants: the Nijmegen cochlear implant questionnaire. Otolaryngol Head Neck Surg 123(6):756–765. https://doi.org/10.1067/mhn.2000.108203
Lin X-J, Lin IM, Fan S-Y (2012) Methodological issues in measuring health-related quality of life. Tzu Chi Med J. https://doi.org/10.1016/j.tcmj.2012.09.002
Patrick DL, Deyo RA (1989) Generic and disease-specific measures in assessing health status and quality of life. Med Care 27(3 Suppl):S217-232. https://doi.org/10.1097/00005650-198903001-00018
Andries E, Gilles A, Topsakal V, Vanderveken Olivier M, Van de Heyning P, Van Rompaey V, Mertens G (2020) Systematic review of quality of life assessments after cochlear implantation in older adults. Audiol Neurotol. https://doi.org/10.1159/000508433
Horsman J, Furlong W, Feeny D, Torrance G (2003) The Health Utilities Index (HUI ® ): concepts, measurement properties and applications. Health Qual Life Outcomes 1:54–54. https://doi.org/10.1186/1477-7525-1-54
Kind P (1996) The EuroQol instrument: an index of health-related quality of life. Quality of life and pharmacoeconomics in clinical trials, 2nd edn. Lippincott-Raven, Philadelphia
Horsman JR, Furlong WJ, Feeny DH, Torrance G (2013) PRM117 - Health Utilities Index (Hui®): Population reference statistics. Value in Health 16(7):A595–A595. https://doi.org/10.1016/j.jval.2013.08.1670
Boyle MH, Torrance GW, Sinclair JC, Horwood SP (1983) Economic evaluation of neonatal intensive care of very-low-birth-weight infants. N Engl J Med 308(22):1330–1337. https://doi.org/10.1056/NEJM198306023082206
Torrance GW, Boyle MH, Horwood SP (1982) Application of multi-attribute utility theory to measure social preferences for health states. Oper Res 30(6):1043–1069. https://doi.org/10.1287/opre.30.6.1043
Halpern SD, Bradley CS, Ming ME, Yang YX (2001) Reliability of the health utilities index—Mark 2 and its applicability to survivors of orthotopic liver transplantation. Liver Transpl 7(3):282–283. https://doi.org/10.1002/lt.500070320
Tonmukayakul U, Le LK, Mudiyanselage SB, Engel L, Bucholc J, Mulhern B, Carter R, Mihalopoulos C (2018) A systematic review of utility values in children with cerebral palsy. Qual Life Res 28(1):1–12. https://doi.org/10.1007/s11136-018-1955-8
Furlong WJ, Feeny DH, Torrance GW, Barr RD (2001) The Health Utilities Index (HUI®) system for assessing health-related quality of life in clinical studies. Ann Med 33(5):375–384. https://doi.org/10.3109/07853890109002092
Crowson MG, Semenov YR, Tucci DL, Niparko JK (2018) Quality of life and cost-effectiveness of cochlear implants: a narrative review. Audiol Neurotol 22(4–5):236–258. https://doi.org/10.1159/000481767
Bond M, Mealing S, Anderson R, Elston J, Weiner G, Taylor RS, Hoyle M, Liu Z, Price A, Stein K (2009) The effectiveness and cost-effectiveness of cochlear implants for severe to profound deafness in children and adults: a systematic review and economic model. Health Technol Assess (Winchester, England) 13(44):1–330. https://doi.org/10.3310/hta13440
Francis HW, Chee N, Yeagle J, Cheng A, Niparko JK (2002) Impact of cochlear implants on the functional health status of older adults. Laryngoscope 112(8):1482–1488. https://doi.org/10.1097/00005537-200208000-00028
Lenarz T, Muller L, Czerniejewska-Wolska H, Valles Varela H, Orus Dotu C, Durko M, Huarte Irujo A, Piszczatowski B, Zadrozniak M, Irwin C, Graham PL, Wyss J (2017) Patient-related benefits for adults with cochlear implantation: a multicultural longitudinal observational study. Audiol Neurootol 22(2):61–73. https://doi.org/10.1159/000477533
Arnoldner C, Lin VY, Bresler R, Kaider A, Kuthubutheen J, Shipp D, Chen JM (2014) Quality of life in cochlear implantees: comparing utility values obtained through the Medical Outcome Study Short-Form Survey-6D and the Health Utility Index Mark 3. Laryngoscope 124(11):2586–2590. https://doi.org/10.1002/lary.24648
McRackan RT, Bauschard LM, Hatch RJ, Franko-Tobin AE, Droghini AH, Velozo RC, Nguyen RS, Dubno RJ (2018) Meta-analysis of cochlear implantation outcomes evaluated with general health-related patient-reported outcome measures. Otol Neurotol 39(1):29–36. https://doi.org/10.1097/MAO.0000000000001620
Gallacher J, Ilubaera V, Ben-Shlomo Y, Bayer A, Fish M, Babisch W, Elwood P (2012) Auditory threshold, phonologic demand, and incident dementia. Neurology 79(15):1583–1590. https://doi.org/10.1212/WNL.0b013e31826e263d
Wouters J, Bosman AJ, Damman W (1995) Realisatie van een CD voor spraakaudiometrie in Vlaanderen. Logopedie En Foniatrie: Maandblad Van De Nederlandse Vereniging Voor Logopedie En Foniatrie 67(9):218–255
van Wieringen A, Wouters J (2008) LIST and LINT: sentences and numbers for quantifying speech understanding in severely impaired listeners for Flanders and the Netherlands. Int J Audiol 47(6):348–355. https://doi.org/10.1080/14992020801895144
Stappen AVD (2000) Computerized electronystagmography: normative data revisited. Acta Otolaryngol 120(6):724–730. https://doi.org/10.1080/000164800750000243
Lazard DS, Vincent C, Venail F, Van de Heyning P, Truy E, Sterkers O, Skarzynski PH, Skarzynski H, Schauwers K, O’Leary S, Mawman D, Maat B, Kleine-Punte A, Huber AM, Green K, Govaerts PJ, Fraysse B, Dowell R, Dillier N, Burke E, Beynon A, Bergeron F, Baskent D, Artieres F, Blamey PJ (2012) Pre-, per- and postoperative factors affecting performance of postlinguistically deaf adults using cochlear implants: a new conceptual model over time. PLoS ONE 7(11):e48739. https://doi.org/10.1371/journal.pone.0048739
Sun DQ, Ward BK, Semenov YR (2014) Bilateral vestibular deficiency: quality of life and economic implications (Report). JAMA Otolaryngol Head Neck Surg 140(6):527. https://doi.org/10.1001/jamaoto.2014.490
Contrera KJ, Betz J, Deal J, Choi JS, Ayonayon HN, Harris T, Helzner E, Martin KR, Mehta K, Pratt S, Rubin SM, Satterfield S, Yaffe K, Simonsick EM, Lin FR (2016) Association of hearing impairment and anxiety in older adults. J Aging Health 29(1):172–184. https://doi.org/10.1177/0898264316634571
Acar B, Yurekli MF, Babademez MA, Karabulut H, Karasen RM (2011) Effects of hearing aids on cognitive functions and depressive signs in elderly people. Arch Gerontol Geriatr 52(3):250–252. https://doi.org/10.1016/j.archger.2010.04.013
Lenarz T, Muller L, Czerniejewska-Wolska H, Vallés Varela H, Orús Dotú C, Durko M, Huarte Irujo A, Piszczatowski B, Zadrożniak M, Irwin C, Graham PL, Wyss J (2017) Patient-related benefits for adults with cochlear implantation: a multicultural longitudinal observational study. Audiol Neurootol 22(2):61–73. https://doi.org/10.1159/000477533
McRackan TR, Bauschard M, Hatch JL, Franko-Tobin E, Droghini HR, Nguyen SA, Dubno JR (2018) Meta-analysis of quality-of-life improvement after cochlear implantation and associations with speech recognition abilities. Laryngoscope 128(4):982–990. https://doi.org/10.1002/lary.26738
Mollenkopf H, Walker A (2007) Quality of life in old age: international and multi-disciplinary perspectives, 1st edn. Springer, Dordrecht
Noble W, Jensen NS, Naylor G, Bhullar N, Akeroyd MA (2013) A short form of the speech, spatial and qualities of hearing scale suitable for clinical use: the SSQ12. Int J Audiol 52(6):409–412. https://doi.org/10.3109/14992027.2013.781278
Gatehouse S, Noble W (2004) The speech, spatial and qualities of hearing scale (SSQ). Int J Audiol 43(2):85–99
Cox MR, Alexander CG (1995) The abbreviated profile of hearing aid benefit. Ear Hear 16(2):176–186. https://doi.org/10.1097/00003446-199504000-00005
McRackan T, Velozo C, Holcomb M, Camposeo E, Hatch J, Meyer T, Lambert P, Melvin C, Dubno J (2017) Use of adult patient focus groups to develop the initial item bank for a cochlear implant quality-of-life instrument. JAMA Otolaryngol Head Neck Surg 143(10):975. https://doi.org/10.1001/jamaoto.2017.1182
McRackan T, Hand B, Velozo C, Dubno J (2019) Cochlear implant quality of life (CIQOL): development of a profile instrument (CIQOL-35 Profile) and a global measure (CIQOL-10 Global). J Speech Lang Hear Res Online 62(9):3554–3563. https://doi.org/10.1044/2019_JSLHR-H-19-0142
EUnetHTA (2015) Endpoints used for relative effectiveness assessment: health-related quality of life and utility measures. https://www.eunethta.eu/wp-content/uploads/2018/01/Endpoints-used-for-Relative-Effectiveness-Assessment-Health-related-quality-of-life-and-utility-measures_Amended-JA1-Guideline_Final-Nov-2015.pdf
Funding
The Antwerp University Hospital currently receives a research grant from the company MED-EL, Innsbruck (Austria).
Author information
Authors and Affiliations
Contributions
EA undertook data collection and analysis and drafted the manuscript. AG, VT, OV, PVDH, VVR and GM critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Consent to participate
All participants gave written informed consent prior to participation in accordance with the Declaration of Helsinki.
Consent for publication
Patients signed informed consent regarding using their data to write and publish this article.
Ethics approval
The study was carried out in conformity with the recommendations of the ethics committee of the University of Antwerp, Antwerp, Belgium and he University Hospital Antwerp, Antwerp, Belgium and the Declaration of Helsinki. The protocols for the control group and the CI users were approved on November 21, 2016 (protocol number: 16/43/450) and June 15, 2015 (protocol number: 15/17/181) respectively.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Andries, E., Gilles, A., Topsakal, V. et al. The impact of cochlear implantation on health-related quality of life in older adults, measured with the Health Utilities Index Mark 2 and Mark 3. Eur Arch Otorhinolaryngol 279, 739–750 (2022). https://doi.org/10.1007/s00405-021-06727-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-06727-3